Why is body composition analysis an effective tool for lymphedema specialists?
Lymphedema is a poorly understood condition characterized by chronic swelling in one or more areas of the body due to impaired lymphatic flow. Secondary lymphedema commonly occurs after cancer treatment or surgery, making it crucial to monitor patients undergoing cancer therapies as lymphedema is commonly underdiagnosed until the edema progresses. Although there is no cure, early detection is key to managing symptoms and progression of lymphedema as well as improving patient outcomes and quality of life.
Lymphedema specialists are responsible for identifying, treating, and monitoring the disease while educating each patient on lifelong self-care. Because lymphedema is not well understood, there are limited tools available to clinicians for providing the best care for their patients. The InBody is a medical-grade bio impedance device that measures body water and composition, providing objective measures of fluid and muscle-fat balance. The InBody test is non-invasive and convenient, and the comprehensive results sheet is the perfect educational tool to engage patients and help them understand more about their condition while using the information to document progress and guide treatments.
In less than 60 seconds, the InBody Test provides accurate, objective, and easily understandable measurements to evaluate the patient’s current health status and track the efficacy of treatments and interventions. Lymphedema specialists can use the InBody to:
- Monitor body water and composition for early detection and treatment of lymphedema
- Identify fluid imbalances through tracking segmental body water values and edema index variables
- Evaluate additional health risks related to muscle-fat balance
Empowered by objective data, clinicians will be able to more effectively identify, treat and manage lymphedema, improving the success of patients and their programs.
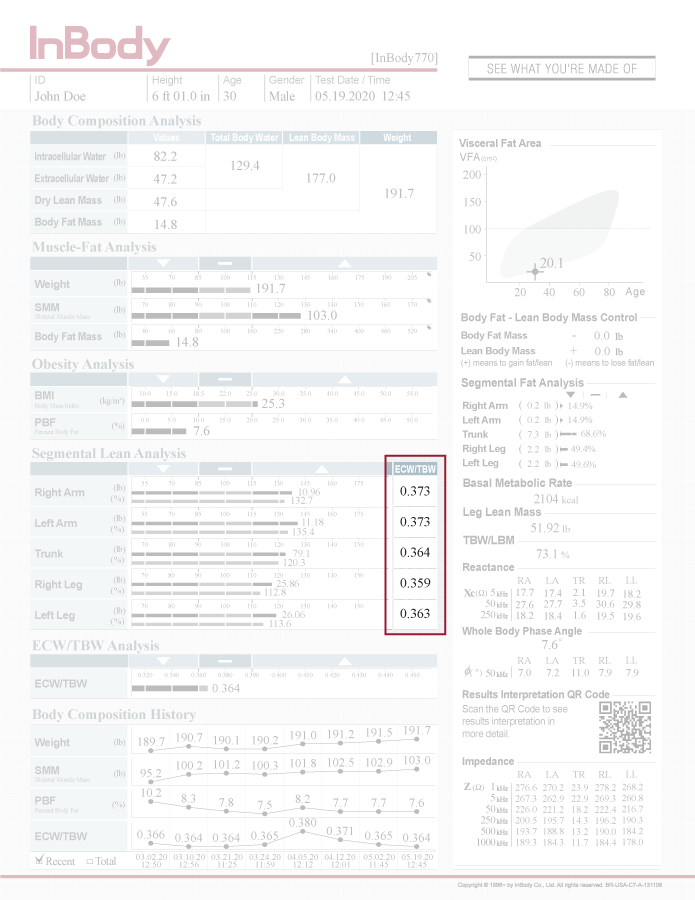
SEGMENTAL BODY WATER ANALYSIS
Detect fluid imbalances resulting from the development or progression of lymphedema
Indirect methods of quantifying body water make it difficult to diagnose and track lymphedema progression. Circumference and perometry measures are commonly used; however, these methods can be time-consuming, prone to error and may not accurately reflect changes in body water.
InBody objectively measures each region of the body separately and provides fluid balance measures for each of the arms, legs and the trunk. This allows clinicians to easily identify both unilateral and bilateral lymphedema as well as monitor changes over time.
Circumference measures and perometry are two methods often used to determine limb volume in order to identify edematous limbs or track lymphedema progression. However, circumference measures suffer from high inter-measurer variability, and certain patients may be excluded from assessment with a perometer. In addition, these indirect volume measurements are often unreliable and do not always reflect changes in body water. For example, changes in lean or fat mass can confound changes that might appear to be (or even mask) swelling. Therefore, it is important for lymphedema specialists to have objective measures of body water for accurate diagnosis and tracking of lymphedema.
InBody effectively distinguishes water in the intracellular (ICW; within the tissues) and extracellular (ECW; within the blood and interstitial fluids) water compartments that comprise total body water. The Edema Index, based on the ratio between ECW and TBW (ECW/TBW), can be used to detect fluid imbalances resulting from the development or progression of lymphedema. This index is provided separately for each arm, leg, and trunk, therefore providing a direct assessment/tracking tool for both edema by avoiding the use of comparisons to unaffected body segments.
The comprehensive body water report provided by the InBody allows objective tracking of fluid balance to help diagnose both unilateral and bilateral lymphedema and effectively monitor patients over time.
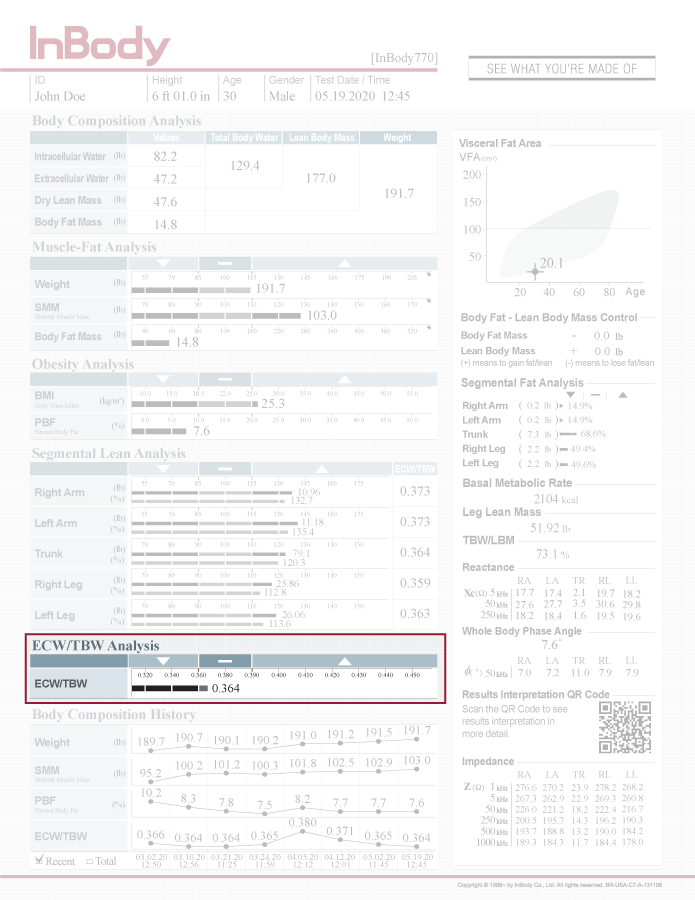
ECW/TBW ANALYSIS
Identify progression of lymphedema early on to increase treatment success
Patient care and management of symptoms become more difficult as lymphedema progresses. Although early detection improves long-term patient outcomes, delayed diagnosis and the limited availability of tools to detect lymphedema often prevent early treatment strategies.
In patients at risk for developing lymphedema, surveillance is key. InBody offers a quick, convenient and non-invasive way to monitor patients preoperatively as well as throughout their treatment programs for earlier detection and treatment of fluid accumulation.
Lymphedema is a common side effect of breast cancer treatment and some surgical procedures yet remains undiagnosed until edema symptoms progress to later stages. It is important to identify lymphedema early in order to prevent progression and preserve the patient’s quality of life. Surveillance and implementation of a tool to non-invasively and effectively monitor patients at risk of developing lymphedema can greatly reduce incidence and aid in the successful management of lymphedema.
InBody uses multiple frequencies and direct segmental measurements for precise and accurate assessment of body water in each arm, leg, and the trunk separately. Changes in ECW/TBW reflect altered fluid balance, and segmental ICW and ECW values can be evaluated to determine whether they are a result of changes in body composition or progression of lymphedema. Segmental phase angle, a representation of cell membrane integrity, can also be tracked to assess patients’ health status. These objective values allow clinicians to detect subclinical changes in fluid accumulation, which allows earlier identification and treatment, increasing patients’ long-term treatment success and quality of life.
BODY COMPOSITION HISTORY
Track trends in patient progress over time
It is often difficult to evaluate treatments (massage therapy, compression, surgery) aimed at promoting lymphatic flow.
The InBody objectively tracks changes in fluid balance, which can be used to determine the effectiveness of different treatments. This data can be utilized to confirm program efficacy and tailor care to the individual, reducing the risk of progression to further stages of lymphedema and/or fibrosis.
As lymphedema progresses, mobility issues and the development of fibrotic tissue causes the quality of life to deteriorate. The development of conditions such as fibrosis can cause increased pain and hinder activities of daily living. Tracking the effects of treatment programs for each patient helps identify successful strategies to promote lymphatic flow and prevent progression to later stages. To do this, a non-invasive and convenient method is necessary to document patients throughout their programs while providing easily comprehensible data to inform both patient and provider.
InBody’s precise water measures reflect changes in lymphedema status as patients undergo different treatment modalities. Whether the patient is undergoing surgery or complete decongestive therapy, obtaining baseline measures and monitoring changes in ECW/TBW over time provides valuable information about how the treatment is improving symptoms. This increases the likelihood of success as clinicians can track which treatments are best suited for each individual and tailor programs according to patients’ needs, thereby improving patient satisfaction, compliance, and long-term outcomes.

SEGMENTAL WATER ANALYSIS
Measure truncal edema in addition to limbs
Truncal edema, whether in the breast or as a byproduct of the lymph edematous limb(s), is common but almost impossible to quantify. InBody measures the trunk region separately, allowing truncal edema to be monitored closely with objective data to develop an appropriate treatment program.
Though lymphedema most clearly presents in the affected limb, lymphatics in the trunk also tend to become imbalanced, causing edema to manifest in the trunk. In most cases, truncal lymphedema is identified indirectly through subjective assessment and physical examination. However, tracking progress or improvement remains a challenge.
InBody uses direct segmental technology to measure the trunk separately, providing objective measures of ICW, ECW and ECW/TBW in this specific segment of the body. The ECW/TBW can be used to identify truncal fluid imbalance, and monitoring truncal ICW and ECW will allow clinicians to determine the cause of any changes, whether stemming from loss of muscle or buildup of fluid. In addition, the efficacy of different treatment modalities, such as manual lymph drainage, compression, and self-care, can be evaluated in order to optimize outcomes while balancing the patient’s unique needs and lifestyle.
Equipped with objective data on body water in the trunk in addition to the limbs, clinicians will be able to make better, more informed decisions to treat lymphedema, and both patient and provider will have a deeper understanding of the body’s response to treatment as well as the physiological changes associated with lymphedema.

